- HOME
- PSYCH SERVICES
- BUSINESS & PERFORMANCE PSYCHOLOGY
- CLINICAL, COUPLES, & FAMILIES
- ADHD Treatment & Evaluation Services
- Anger Management
- Anxiety Treatment & Evaluation Services
- Borderline Personality Treatment Services
- Cognitive Behavioral Therapy (CBT) Self-Help
- Couples Counseling and Marital Therapy
- Consent for Psychological Services for Minors Post-Divorce
- Depression Treatment Services
- Infidelity Recovery
- Jacksonville Counseling and Psychology
- Military Psychology & Tricare
- Narcissistic Personality Treatment Services
- Online Counseling
- Psychoeducational Testing
- Psychological Testing and Assessment
- Psychotherapy & Counseling
- FORENSIC PSYCHOLOGY & EXPERT TESTIMONY
- LIFE COACHING & EXECUTIVE COACHING
- PSYCHOLOGICAL PUBLIC DISABILITY QUESTIONNAIRES (DBQ)
- ONLINE COURSES
- Our Partnership Begins When You Purchase an Online Course
- Get to Know Dr. D’Arienzo, Relationship Expert
- Florida Premarital Preparation Online Course
- Georgia Premarital Education Online Course
- TwogetherinTexas Premarital Online Course
- Tennessee Premarital Preparation Online Course
- Minnesota Premarital Education Course Online
- Oklahoma Premarital Counseling Online Course
- South Carolina Premarital Preparation Course
- West Virginia Premarital Education Course
- Online Marriage and Relationship Tune Up Course
- Florida DCF Certified Parent Education and Family Stabilization Online Course
- Georgia Qualified Parent Education and Family Stabilization Online Course
- Texas Qualified Parent Education and Family Stabilization Online Course
- High Conflict Co-Parenting Online Certificate Course (8 Hours)
- Online Anger Management Four Hour Course (Level 1)
- Online Anger Management Eight Hour Course (Level 2)
- Sexual Harassment Online Training
- MMPI/GUARD/LEO
- CPI Police and Public Safety Assessment
- G License Psychological Testing
- Online Psychological Testing for Armed Security Guards and Personal Protection Officers
- MMPI Texas Level III CSO and IV PPO Psychological (ONLINE)
- Requirement for Texas Security License Applicants: MMPI Evaluation
- Level 3 Security Guard New Mexico Online MMPI Psychological Evaluation
- TEAM
- SOCIAL MEDIA/BOOKS
Biden Anxiety and Dementia
Posted by: Dr. Justin D'Arienzo, Psy.D., ABPP
Biden Anxiety and Dementia
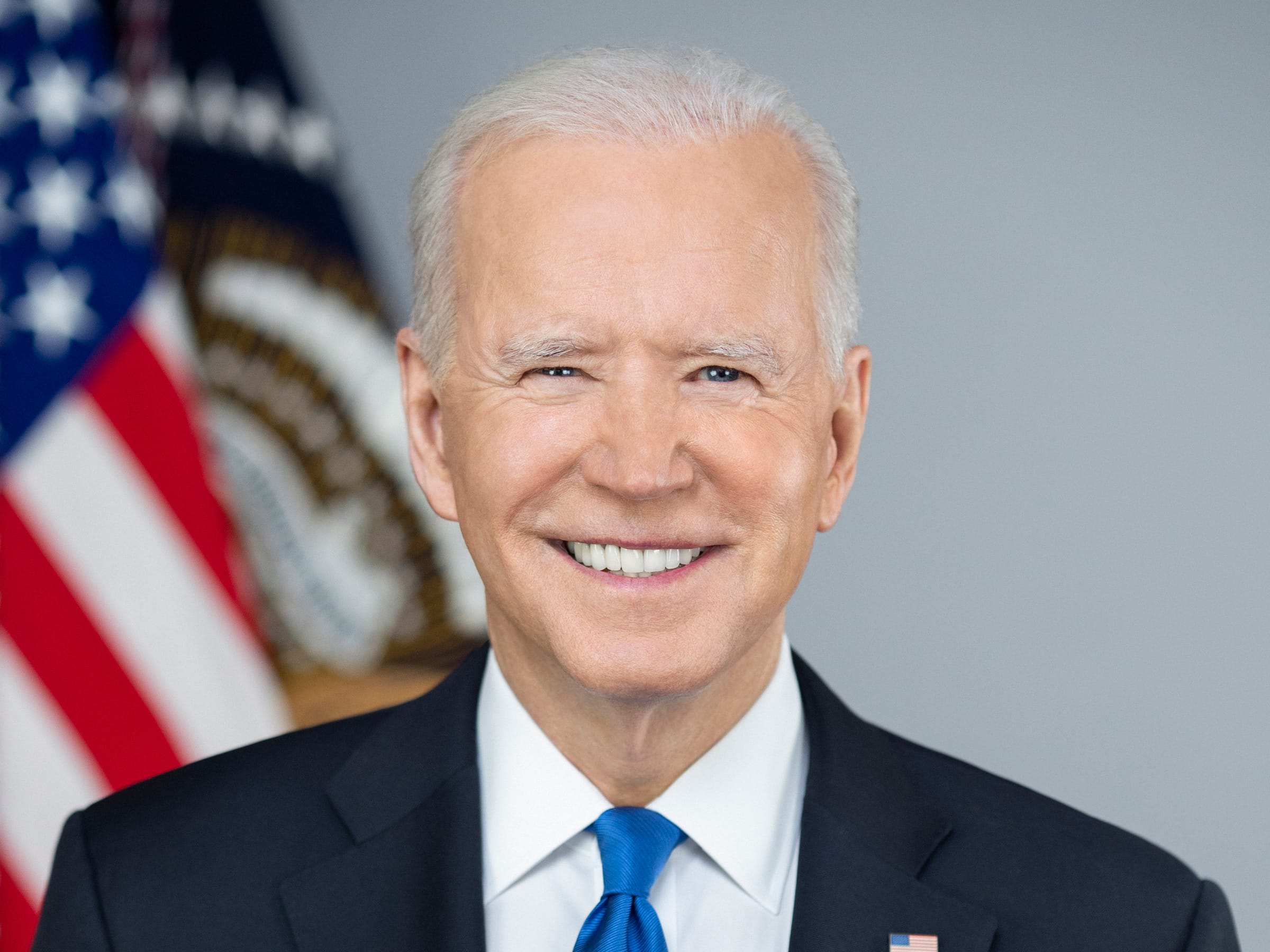
Whether Republican or Democrat, President Joe Biden’s behavior on camera is concerning to most causing anxiety about whether he should either be the Democratic candidate or about who Former President, Donald Trump, will be running against in November 2024. It’s also concerning that Biden may have lost insight about his own abilities due to his cognitive decline. As a public service announcement, I have provided information below about dementia as well as the lack of insight into one’s own symptoms that often accompanies dementia and other cognitive disorders. Then, I discuss the difference between dementia and the normal aging process. It should also be noted that neuropsychologists and other psychologists administer cognitive tests and assessments for those with dementia and for those who are candidates for certain occupations like law enforcement, nuclear, special forces or leadership roles within companies. Many have heard both recent presidents tout taking the Montreal Cognitive Assessment (MoCA). This is a simple screening assessment and not a diagnostic tool. It is only the beginning of a neuropsychological and cognitive testing assessment.
The DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, 5th Edition) outlines the diagnostic criteria for Major Neurocognitive Disorder (NCD), commonly referred to as dementia. The symptoms and criteria include:
- Significant Cognitive Decline: Evidence of significant cognitive decline from a previous level of performance in one or more cognitive domains (complex attention, executive function, learning and memory, language, perceptual-motor, or social cognition) based on:
- Concern of the individual, a knowledgeable informant, or the clinician that there has been a significant decline in cognitive function; and
- A substantial impairment in cognitive performance, preferably documented by standardized neuropsychological testing, or, in its absence, another quantified clinical assessment.
- Interference with Independence: The cognitive deficits interfere with independence in everyday activities (i.e., requiring assistance with complex instrumental activities of daily living, such as paying bills or managing medications).
- Not Delirium: The cognitive deficits do not occur exclusively in the context of a delirium.
- Not Better Explained by Another Disorder: The cognitive deficits are not better explained by another mental disorder (e.g., major depressive disorder, schizophrenia).
The DSM-5 also specifies subtypes of Major Neurocognitive Disorder based on etiology, such as Alzheimer’s disease, vascular disease, traumatic brain injury, substance/medication use, HIV infection, prion disease, Parkinson’s disease, Huntington’s disease, and others. Each subtype has additional specific criteria related to the underlying cause.
DSM-5-TR Criteria for Dementia
The DSM-5-TR outlines specific criteria for diagnosing Major Neurocognitive Disorder, which is commonly referred to as dementia. The core features include:
- Significant Cognitive Decline: This is evidenced by a noticeable decline from previous levels of performance in one or more cognitive domains. These domains include complex attention, executive function, learning and memory, language, perceptual-motor, and social cognition. The decline must be substantiated by:
- Concern from the individual, a knowledgeable informant, or the clinician about a significant deterioration in cognitive abilities.
- Substantial impairment in cognitive performance, ideally documented through standardized neuropsychological testing or another quantified clinical assessment.
- Interference with Independence: The cognitive deficits must interfere with the individual’s independence in daily activities. This typically involves needing help with complex instrumental activities such as managing finances or medications.
- Exclusion of Delirium: The cognitive deficits must not occur exclusively during episodes of delirium.
- Exclusion of Other Mental Disorders: The cognitive deficits should not be better explained by another mental disorder, such as major depressive disorder or schizophrenia.
Lack of Insight (Anosognosia) in Dementia
An often-overlooked but significant symptom of dementia is anosognosia, or poor insight into one’s cognitive impairments. Anosognosia refers to a person’s inability to recognize the extent of their deficits, which can severely impact their care and treatment.
In the context of dementia, lack of insight manifests as a diminished awareness of cognitive decline. This can result from damage to brain regions responsible for self-awareness, particularly the frontal and parietal lobes. As these areas deteriorate, individuals may lose the ability to accurately assess their cognitive state.
Impact of Poor Insight on Diagnosis and Management
Poor insight into one’s condition poses several challenges in diagnosing and managing dementia:
- Delayed Diagnosis: Individuals with anosognosia may not seek medical help early, as they fail to recognize their symptoms. This can delay diagnosis and intervention, allowing the disease to progress unchecked.
- Compliance Issues: Lack of awareness can lead to non-compliance with treatment regimens. Patients may forget to take medications, attend appointments, or follow therapeutic recommendations, which can exacerbate their condition.
- Safety Concerns: Poor insight increases the risk of dangerous behaviors, such as driving with impaired abilities, mishandling finances, or neglecting personal care. This not only endangers the individual but also places a burden on caregivers.
- Caregiver Strain: Family members and caregivers often face significant stress when dealing with a loved one who does not recognize their cognitive decline. This can lead to frustration, strained relationships, and burnout.
Addressing Anosognosia in Dementia Care
Effective management of dementia requires addressing anosognosia. Here are some strategies:
- Education and Support: Educating patients and caregivers about anosognosia can help manage expectations and reduce frustration. Support groups and counseling can provide emotional relief and practical advice.
- Routine Assessments: Regular cognitive assessments can help track the progression of dementia and adjust care plans accordingly. Clinicians should consider incorporating tools that evaluate insight as part of these assessments.
- Safety Measures: Implementing safety measures, such as supervised activities, financial oversight, and home modifications, can mitigate the risks associated with poor insight.
- Caregiver Training: Training caregivers in communication strategies and coping techniques can improve their ability to manage challenging behaviors linked to anosognosia.
Conclusion
Diagnosing dementia involves recognizing a range of cognitive deficits as outlined in the DSM-5-TR criteria. Anosognosia, or poor insight into one’s cognitive decline, is a critical symptom that complicates diagnosis and management. By understanding and addressing this symptom, healthcare providers can improve care outcomes and enhance the quality of life for individuals with dementia and their caregivers. Early diagnosis, routine assessments, and comprehensive support systems are essential in effectively managing this challenging condition.
The Role of Neuropsychologists in Diagnosing Dementia
Neuropsychologists play a crucial role in diagnosing dementia, providing detailed assessments and insights that are integral to understanding and managing this complex condition. Their expertise lies in evaluating cognitive functions, identifying specific deficits, and differentiating dementia from other neurological and psychiatric disorders.
Comprehensive Cognitive Assessments
One of the primary roles of neuropsychologists in diagnosing dementia is conducting comprehensive cognitive assessments. These assessments involve a battery of standardized tests designed to evaluate various cognitive domains, such as memory, attention, language, executive function, and visuospatial abilities. By systematically examining these areas, neuropsychologists can pinpoint specific impairments that are characteristic of different types of dementia.
Differential Diagnosis
Dementia can be challenging to diagnose due to its symptom overlap with other conditions, such as depression, mild cognitive impairment (MCI), and other neurodegenerative diseases. Neuropsychologists use their expertise to differentiate dementia from these conditions through careful analysis of test results, clinical history, and symptom patterns. This differential diagnosis is essential for ensuring accurate treatment and management plans.
Baseline and Longitudinal Evaluations
Neuropsychologists often establish a cognitive baseline for patients, which serves as a reference point for tracking changes over time. Longitudinal evaluations are critical in monitoring the progression of dementia and adjusting care plans accordingly. By comparing current cognitive performance with baseline data, neuropsychologists can detect subtle changes that might indicate the onset or progression of dementia.
Identifying Specific Dementia Subtypes
Different types of dementia, such as Alzheimer’s disease, vascular dementia, Lewy body dementia, and frontotemporal dementia, have distinct cognitive profiles. Neuropsychologists are trained to recognize these profiles and identify the specific subtype of dementia. This identification is crucial for tailoring treatment strategies, as each subtype may respond differently to various interventions.
Assessing Insight and Awareness
As discussed, lack of insight, or anosognosia, is a common symptom of dementia. Neuropsychologists assess patients’ awareness of their cognitive deficits, which can significantly impact treatment compliance and safety. Understanding the extent of a patient’s insight helps in designing appropriate interventions and providing education and support to caregivers.
Recommending Interventions and Support
Based on their assessments, neuropsychologists provide detailed recommendations for interventions and support. These may include cognitive rehabilitation, behavioral strategies, and environmental modifications to enhance safety and independence. They also offer guidance on managing challenging behaviors and improving the quality of life for both patients and caregivers.
Collaborative Approach
Neuropsychologists often work as part of a multidisciplinary team, collaborating with neurologists, psychiatrists, primary care physicians, and other healthcare professionals. This collaborative approach ensures a comprehensive evaluation and management plan, addressing the medical, psychological, and social aspects of dementia care.
Educating Patients and Caregivers
Education is a vital component of a neuropsychologist’s role. They provide patients and caregivers with information about the nature of dementia, expected progression, and strategies for managing symptoms. This education helps in setting realistic expectations and reducing anxiety and stress associated with the diagnosis.
Research and Advancements
Neuropsychologists also contribute to the field of dementia through research. They investigate cognitive functioning, develop new assessment tools, and explore innovative treatment approaches. Their research efforts enhance understanding of dementia and contribute to improved diagnostic and therapeutic techniques.
Conclusion
Neuropsychologists are essential in diagnosing dementia, offering comprehensive assessments, differential diagnoses, and tailored recommendations. Their expertise ensures accurate identification of cognitive deficits, aiding in the effective management of dementia. By working collaboratively with other healthcare professionals and providing education and support, neuropsychologists play a pivotal role in enhancing the quality of life for individuals with dementia and their caregivers.
Understanding Normal Aging Process vs. Dementia
As individuals age, certain changes in cognitive abilities and brain function are expected. However, distinguishing these normal age-related changes from the symptoms of dementia is crucial for proper diagnosis and intervention. Here, we explore the differences between the normal aging process and dementia.
Normal Aging Process
The normal aging process involves gradual changes in cognitive function and brain structure. These changes are typically mild and do not significantly interfere with daily activities or quality of life.
Key Characteristics of Normal Aging:
- Memory:
- Occasional forgetfulness, such as misplacing items or forgetting names, but remembering them later.
- Slower recall of names, dates, and events.
- Attention and Processing Speed:
- Slight decline in the ability to maintain focus for extended periods.
- Slower processing of information and reaction times.
- Executive Function:
- Mild difficulties in multitasking or quickly switching between tasks.
- Slight challenges in problem-solving or decision-making.
- Language:
- Occasional difficulty finding the right word, but ability to carry on conversations and understand instructions remains intact.
- Visuospatial Skills:
- Minor difficulties with spatial orientation, such as judging distances or navigating new places.
- Independence:
- Ability to perform daily activities and maintain independence remains largely unaffected.
Dementia
Dementia is a collective term for a range of neurocognitive disorders characterized by significant cognitive decline that interferes with daily life and activities. The decline is more severe than what is expected from normal aging and often includes multiple cognitive domains.
Key Characteristics of Dementia:
- Memory:
- Significant and persistent memory loss, particularly for recent events and new information.
- Frequent repetition of questions or stories and reliance on memory aids.
- Attention and Processing Speed:
- Noticeable difficulty in maintaining focus and severe slowing in processing information.
- Easily distracted and difficulty completing tasks.
- Executive Function:
- Substantial impairment in planning, organizing, and problem-solving.
- Inability to manage finances, medications, or complex tasks.
- Language:
- Pronounced difficulties in finding words, following conversations, and understanding spoken or written language.
- Frequent pauses and less coherent speech.
- Visuospatial Skills:
- Severe difficulties with spatial orientation, leading to getting lost in familiar places.
- Problems with recognizing faces, objects, or interpreting visual information.
- Independence:
- Loss of ability to perform daily activities independently, such as dressing, bathing, or eating.
- Increased reliance on caregivers for basic needs.
Differentiating Normal Aging from Dementia
Understanding the differences between normal aging and dementia involves recognizing the severity and impact of cognitive changes. While normal aging includes minor cognitive declines that do not interfere significantly with daily life, dementia involves profound impairments that disrupt independent functioning.
Evaluation and Diagnosis:
- Medical History and Physical Examination: A thorough review of medical history and a physical exam to rule out other conditions.
- Cognitive Testing: Tools like the MoCA and MMSE screen for deficits and other neuropsychological assessments help quantify cognitive deficits and identify dysfunctional brain regions.
- Imaging and Laboratory Tests: Brain imaging (MRI, CT scans) and blood tests to identify underlying causes and rule out other conditions.
- Functional Assessment: Evaluating the individual’s ability to perform daily activities and maintain independence.
Conclusion
Distinguishing between the normal aging process and dementia is essential for appropriate care and intervention. While normal aging involves mild cognitive changes that do not significantly disrupt daily life, dementia is marked by severe cognitive impairments that interfere with independence and quality of life. Proper evaluation and diagnosis by healthcare professionals, including neuropsychologists, are crucial in managing and supporting individuals experiencing cognitive decline.
Categories
- Business Psychologist (4)
- Parent Education and Family Stabilization Course (29)
- School and Child Psychology (15)
- High Conflict Parenting (28)
- Mental Health (61)
- Stress Management (33)
- Sport Psychology (10)
- Counseling Services (54)
- Business Psychologist (24)
- Business Psychologist (12)
- G License Psychological Testing (8)
- Minnesota Premarital Course (10)
- Educational and School Psychology (10)
- Sexual Harassment Training (2)
- Sexual Harassment Training (1)
- Premarital Preparation Courses (7)
- Divorce (14)
- Forensic Psychologist (15)
- Social Media Links (21)
- Alan Lipzin's Posts (5)
- CBT (50)
- Family Law (58)
- Life Coaching (89)
- Marriage Advice (89)
- Military Mental Health (42)
- Psychology and Psychotherapy (134)
- Relationship Advice (80)
- Uncategorized (25)
- TV Appearances (15)
- Premarital Education Courses (46)
- Couples Counseling (51)
- Parenting Coordination (18)
- Bipolar Disorder (5)
- Schizophrenia (3)
- Anger Management (23)
- TwogetherinTexas (8)
Latest News
- September 16th, 2025Do we need premarital counseling?
- September 5th, 2025Empowering Texas School Safety
- September 2nd, 2025Florida Premarital Preparation Course Psychologist
- August 19th, 2025Learning to Manage Conflict with our Florida Premarital Preparation Course
- August 5th, 2025Information about Florida Online Premarital Course and Premarital Counseling
- View All News